TIM-3 therapy for Alzheimer’s disease is emerging as a groundbreaking approach in the quest for effective treatments for this debilitating condition. Focusing on the role of the immune system’s checkpoint molecules, this innovative strategy reawakens the brain’s immune cells, known as microglia, to target and clear amyloid plaques responsible for cognitive decline. Research has shown that inhibiting TIM-3 allows these microglia to resume their critical function of plaque removal, leading to improved cognitive function in mouse models. As researchers explore cancer therapy repurposing, this potential shift in Alzheimer’s disease treatment could open doors to new therapeutic strategies that enhance memory and brain health. By altering the behavior of microglia through TIM-3 modulation, we may soon witness a significant advancement in the landscape of Alzheimer’s disease therapies.
The innovative approach of TIM-3 therapy for cognitive decline taps into immunological strategies originally developed for cancer treatments. By targeting the immune checkpoint protein TIM-3, researchers aim to restore the ability of microglia, the brain’s own immune defense, to combat the buildup of harmful amyloid plaques associated with Alzheimer’s. This research highlights a promising path towards enhancing brain health and cognitive function, signaling a potential shift in Alzheimer’s disease treatment paradigms. As scientists continue to investigate the interplay between the immune system and neurodegenerative processes, the prospect of repurposing existing therapies may pave the way for groundbreaking advancements in fighting Alzheimer’s and preserving cognitive abilities. Through these efforts, we may uncover transformative solutions that elevate quality of life for individuals grappling with this challenging disease.
The Connection Between Cancer Therapy and Alzheimer’s Disease
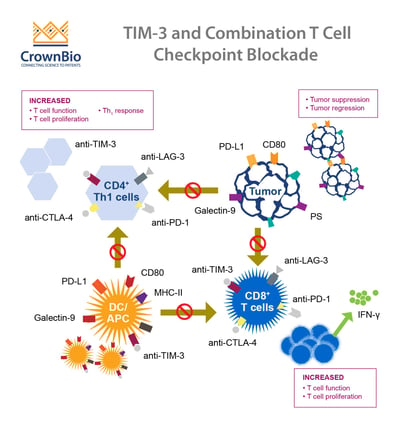
Recent research has highlighted a fascinating connection between cancer therapies, specifically those targeting immune system checkpoint molecules, and potential treatment options for Alzheimer’s disease. This intersection emerges from the understanding of how immune cells function, particularly in relation to TIM-3, an inhibitory checkpoint molecule that plays a crucial role in regulating immune responses in the brain. The ability of these therapies to free microglia — the brain’s resident immune cells — to clear amyloid plaques, which are hallmark features of Alzheimer’s disease, suggests a promising new avenue for cognitive function improvement.
Cancer therapies often aim to enhance the immune response against tumor cells by blocking these checkpoint molecules, thus allowing T cells to function more effectively. Similarly, inhibiting TIM-3 expression in microglia has shown potential in rejuvenating their ability to target and eliminate amyloid plaques in Alzheimer’s disease. This repurposing of cancer treatment methodologies emphasizes the need for integrated research approaches that can utilize successful cancer therapies in the context of neurodegenerative diseases.
Understanding Microglia’s Role in Alzheimer’s Disease
Microglia serve as the primary immune defenders within the brain, and their role is crucial as neuroinflammation has been implicated in the progression of Alzheimer’s disease. As these immune cells encounter amyloid-beta plaques, they are expected to eliminate them; however, increased TIM-3 expression in microglia inhibits their phagocytic actions. This blockage results in plaque accumulation, which is damaging to cognitive function and memory capabilities. Consequently, understanding how TIM-3 modulates microglial activity is vital for exploring new therapeutic avenues.
The dysfunctional behavior of microglia in Alzheimer’s patients can be addressed through strategies involving TIM-3 modulation. By reducing TIM-3’s inhibitory influence, microglia can regain their capacity to clear harmful plaques, potentially leading to significant improvements in cognitive outcomes. This line of research offers a promising strategy, emphasizing the interplay between immune checkpoint regulation and Alzheimer’s disease pathology.
Innovative Approaches in Alzheimer’s Disease Treatment
The evolving landscape of Alzheimer’s disease treatment is witnessing innovative approaches that harness existing knowledge from cancer treatments. The use of TIM-3 therapy represents a new frontier, where strategies initially developed for cancer cell targeting are now being explored for cognitive function restoration. This therapeutic potential demonstrates how interdisciplinary approaches can yield groundbreaking solutions in drug development.
Further exploration of TIM-3 inhibitors, whether through monoclonal antibodies or small molecules, aims to enhance the immune system’s ability to confront the challenges posed by Alzheimer’s. As researchers delve deeper into this uncharted territory, the hope is to develop effective therapies that can mitigate or even halt disease progression, addressing the unmet needs of patients suffering from this debilitating condition.
The Role of TIM-3 in Late-Onset Alzheimer’s
In late-onset Alzheimer’s disease, which accounts for the majority of cases, TIM-3’s critical role may hold the key to understanding disease mechanisms. Genetic associations have identified TIM-3 as a risk factor in Alzheimer’s patients, highlighting its involvement in the disease’s progression. Elevated levels of TIM-3 on microglia may prevent the necessary response to amyloid plaques, resulting in continued neurodegeneration and cognitive decline.
The implications of these findings are profound for therapeutic strategies. By targeting TIM-3, researchers hope to reactivate microglial function to restore their ability to clear amyloid plaques. This potential to modify disease outcomes through a better understanding of late-onset Alzheimer’s pathology could reshape treatment paradigms and foster a new era in Alzheimer’s disease management.
Repurposing Cancer Therapies for Neurodegenerative Diseases
The concept of repurposing cancer therapies for diseases such as Alzheimer’s is gaining traction within the medical research community. This approach recognizes that many treatments developed for one condition may inadvertently benefit another, particularly when those conditions share common biological pathways. By strategically applying immune checkpoint blockade principles from cancer therapy, researchers are paving the way for potential breakthroughs in neurodegenerative disease treatment.
Specifically, existing anti-TIM-3 antibodies used in cancer therapy could potentially be repurposed to address the neuroinflammation seen in Alzheimer’s. This innovative strategy not only accelerates the translational research phase but also presents a more direct method to leverage established safety profiles of these drugs for Alzheimer’s patients, thereby enhancing cognitive function and slowing disease progression.
Exploring Future Directions in Alzheimer’s Research
As research into TIM-3 therapy for Alzheimer’s disease advances, future directions will focus on clinical trials and the evaluation of therapeutic efficacy in human subjects. Recent promising findings in animal models must be translated into effective treatments for patients who suffer from these debilitating cognitive disorders. Interdisciplinary collaborations, like those observed in the recent studies, will be crucial for optimizing therapies and accelerating the path to clinical application.
Emerging clinical trials will likely utilize genetically modified mouse models to test human-compatible anti-TIM-3 antibodies, assessing their impact on amyloid plaque accumulation and cognitive function. The outcomes of these studies could not only enhance our understanding of TIM-3’s role in Alzheimer’s disease but also provide critical insights into the potential for immune checkpoint modulation as a valid therapeutic strategy.
Cognitive Function Improvement Through Immunotherapy
Immunotherapy has emerged as a viable option for improving cognitive function in individuals with Alzheimer’s disease. By focusing on the immune system’s role, particularly the regulation of microglial activity through checkpoint inhibitors like TIM-3, researchers are pioneering new methodologies intended to enhance memory and cognitive capabilities. These advancements signal a shift away from traditional therapeutic approaches that primarily target amyloid plaques.
Studies have shown that alleviating the effects of TIM-3 in microglia can restore their capability to combat plaque accumulation, leading to observable improvements in behavior and cognitive tasks in animal models. This exciting development brings hope not only for better memory retention but also for overall cognitive health, highlighting the need for continued exploration in the realm of immunotherapy for Alzheimer’s disease.
Genetic Insights into Alzheimer’s Disease Risk Factors
Genetic factors play an influential role in the susceptibility to Alzheimer’s disease, particularly in understanding the polymorphisms associated with TIM-3. As researchers investigate the genetic underpinnings of the disease, these insights could pave the way for personalized treatment approaches that target specific genetic configurations in Alzheimer’s patients. This progression in genetic research could significantly alter how treatments are designed, making them more effective based on individual genetic makeups.
The identification of TIM-3 as a genetic risk factor for late-onset Alzheimer’s showcases the importance of integrating genetic analysis into clinical practice. With a deeper understanding of how TIM-3 impacts microglial function and plaque clearance, future therapies can be tailored not only to alleviate symptoms but also to counteract genetic predispositions that may hasten disease progression.
The Importance of Collaborative Research in Alzheimer’s Therapy
Collaboration among researchers from diverse fields is crucial for advancing Alzheimer’s disease therapies. The multidisciplinary team approach has already demonstrated immense potential in studies targeting the immune system and its implications for cognitive function improvement. By combining expertise from neurology, immunology, and genetics, researchers can more effectively tackle the complexities of Alzheimer’s disease and develop innovative treatment strategies.
Through collaborative efforts, researchers can also pool resources and share findings, fostering a community of innovation that accelerates the pace of discovery. The work done by teams exploring TIM-3 therapy not only exemplifies this collaborative spirit but also underscores the need for continued partnership across different scientific disciplines to unravel the complexities of Alzheimer’s and develop effective therapies.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease and how does it work?
TIM-3 therapy for Alzheimer’s disease involves targeting the TIM-3 molecule, which acts as an immune system checkpoint, inhibiting microglia from clearing amyloid plaques in the brain. By blocking TIM-3, microglia can be activated to attack and remove these harmful plaques, potentially improving cognitive function in Alzheimer’s patients.
How does the TIM-3 molecule relate to the immune system and Alzheimer’s disease?
The TIM-3 molecule is an immune checkpoint expressed by microglia, the brain’s immune cells. In Alzheimer’s disease, TIM-3 prevents microglia from effectively clearing amyloid plaques, contributing to the disease’s progression by inhibiting cognitive function improvement.
Can TIM-3 therapy be used alongside existing Alzheimer’s disease treatments?
Yes, TIM-3 therapy for Alzheimer’s disease can be explored in conjunction with existing treatments. Since it focuses on modifying the immune response, it may enhance the effectiveness of other therapies aimed at targeting amyloid plaques.
What are the potential benefits of using TIM-3 therapy for treating Alzheimer’s disease?
The potential benefits of TIM-3 therapy for treating Alzheimer’s disease include enhanced clearance of amyloid plaques by activated microglia, leading to improved cognitive function and memory in patients with Alzheimer’s.
Are there any ongoing clinical trials for TIM-3 therapy aimed at Alzheimer’s disease?
Ongoing research includes testing anti-TIM-3 antibodies in mouse models that mimic Alzheimer’s disease. These studies aim to assess the therapy’s effectiveness before progressing to human clinical trials.
What evidence supports the effectiveness of TIM-3 therapy for Alzheimer’s disease?
Research indicates that genetically modified mice lacking TIM-3 show improved plaque clearance and cognitive behavior. This suggests that TIM-3 therapy may restore normal microglial function, potentially reversing cognitive decline associated with Alzheimer’s.
What is the significance of TIM-3 as a genetic risk factor for Alzheimer’s disease?
TIM-3 has been identified as a genetic risk factor for late-onset Alzheimer’s disease due to its polymorphism in patients, indicating a biological mechanism by which it negatively influences microglial activity in plaque clearance.
What is the next step in developing TIM-3 therapy for human patients with Alzheimer’s disease?
The next step involves exploring the efficacy of human anti-TIM-3 antibodies in mouse models that have incorporated the human TIM-3 gene, paving the way for future clinical applications in Alzheimer’s disease treatment.
How does TIM-3 therapy compare to traditional anti-amyloid therapies for Alzheimer’s disease?
Unlike traditional anti-amyloid therapies that may cause adverse vascular effects, TIM-3 therapy specifically targets the immune response to plaques, offering a potentially safer and more effective approach to treating Alzheimer’s disease.
What is the role of microglia in Alzheimer’s disease and how does TIM-3 influence this?
Microglia play a critical role in clearing amyloid plaques in Alzheimer’s disease. TIM-3 influences microglia by keeping them in a homeostatic state that inhibits plaque clearance, contributing to the worsening of cognitive function in patients.
| Key Points | |
|---|---|
| TIM-3 therapy may improve memory and cognition in Alzheimer’s patients by enhancing microglial activity. | Research shows that blocking TIM-3 allows microglia to attack and clear brain plaques associated with Alzheimer’s disease. |
| A significant percentage (90-95%) of Alzheimer’s cases are late-onset, where TIM-3 is implicated as a genetic risk factor. | Once activated, microglia use TIM-3 to regulate their activity, but in Alzheimer’s, this inhibits their ability to clear harmful plaques. |
| Using lab mice that lack the TIM-3 gene showed enhanced plaque clearance and some cognitive recovery, indicating a potential therapy route. | Research is ongoing to test an anti-TIM-3 antibody’s effectiveness in halting plaque formation in Alzheimer’s models. |
Summary
TIM-3 therapy for Alzheimer’s disease represents a promising new approach to combatting the cognitive decline associated with this devastating illness. By blocking the TIM-3 molecule that inhibits microglial function, researchers have found an innovative way to enable these essential brain immune cells to clear the amyloid plaques that contribute to memory loss and cognitive impairment. Continued research in this area may provide a path toward effective treatments for those affected by Alzheimer’s.